In this episode of the Wolf’s Den I have a discussion with gut health expert, David O’Brien. David gets deep into the nitty-gritty of gut health.
Listen on iTunes or Soundcloud:
Transcript From How To Restore Gut Health | Wolfpack Episode 11 with Dave O’Brien and Mark Ottobre Video
(This transcription may contain errors)
Welcome to the show that entertains and educates. Welcome to the Wolf’s Den. My name is Mark Ottobre, and today’s guest is the co-owner of 5th Element Wellness that recently won the Fitness Independent Business of the year award at the recent Fitness Australia Awards. He’s known around the traps as the “gut guy” and people from all over are coming to see him in droves ’cause of the results that he’s getting for his clients. Please put your hands together and welcome David O’Brien.
Welcome, David.
Thank you very much, Mark.
How’s it going?
Good. Amazing.
The obligatory question.
Yeah. Well, thanks for having me, first.
Oh, absolutely.
It’s amazing to be here. Yeah, so, I’m getting renown for being a bit of an expert on the gut. I think, actually, one of your trainers actually called me the rain man when it actually came to gut, and that’s actually-
That be Tyler Costner.
Yes.
He’s with us today.
Yes, Tyler. Yeah. Who I’ve helped with a bit of gut issues. I might use him as a bit of an example somewhere along the line. But it’s quite funny, actually, because we actually put a survey up when we actually do things like blood chemistry analysis and stool analysis and so forth. And actually, someone actually wrote in there, asking if I had Asperger’s.
It’s kind of a double-handed compliment.
Yeah. I’ll take it.
You’ll take it. Yeah, yeah.
I’ll take it. I don’t have Asperger’s, by the way. Not to my knowledge, unless people think I’ve got Asperger’s. But I might display a little bit of tendencies of Asperger’s.
That’s great. So, you started as a trainer when?
I’ve been a trainer… it’s a long time, actually. Actually, out of university… I actually didn’t practice being a trainer straightaway out of university. Actually, I was doing landscape gardening, believe it or not, which is far away from personal training. But I actually did it to get some money so I could actually go traveling, and it was actually when I went to London that I became a… started practicing my trade. In London, I worked there for 10 years and I actually worked in a few boutique facilities in London, and I actually had a pretty amazing clientele, but I got caught in the rat race in London, to be honest.
I practiced exactly what I sort of learned at university, and I think there’s a lot of limitations in just sort of practicing sort of one formula of how to train people. I found that I was sort of a little bit of a mixed bag. The results I was getting with clients, it was a bit hit and miss. Most of the clients I was working with I was not really getting the impact that I wanted to and just a minute amount I was actually getting some all right results, do you know what I mean?
What year was that?
So, it was 2000 that I went to the UK, and I stayed there for 10 years. But the problem was, and for any aspiring trainers out there, the problem was that I didn’t really further my education for quite a long period of time ’cause I thought I was amazing. I was training, doing 55 sessions in a week, and I thought that was incredible because it was just churn and burn and so forth. But it wasn’t until maybe about five years later that actually someone told be about Charles Poliquin, actually.
It was actually one of my good mates who’s actually one of the head guys in UP, Eduardo Baruta. He actually told me about Charles, and I actually went along to one of Charles’ buy a signature courses. And that was the time, because it was five days and he actually went pretty heavy into biochemistry. He didn’t really touch a huge amount on gut health, but it was a lot on detoxification, micronutrients, and all that. And over those five days, that was the moment I realized I knew nothing.
Five years of doing PT, meet Charles Poliquin, the pioneer, in my opinion, of this industry, changes your direction and course. So I know part of, ’cause I’m a student-I mean, we’re all in the fitness industry, I feel, in some way form and shape students of Charles whether it’s directly or indirectly and things like this. But for you, you did a course with Charles. He put you on a direction. It’s seems although, ’cause there are guys who go in, myself included, different directions, you found the functional medicine side or functional health side of things. How did you find that and when? When did you fall in love with that?
Just quickly, back to Charles, it was actually a conversation that I had with Charles and rest his soul. He was good enough to give me 10 minutes of his time. We actually sat down and I said, “This is some of the thoughts that I’ve got with the fitness industry.” Which was based on more of a holistic model and so forth. But he basically said to me, “All the stuff that I’m teaching you now means nothing unless you actually go away and you research it more than I’ve researched it.” Okay? And it was a conversation that sticks in my head today. I cannot repay the motivation that Charles gave me. Okay?
And actually, I took that literally. Maybe applied a bit of that Asperger’s demeanor. Yeah? And I literally just … when I actually, eventually sort of came back to Australia I literally on weekends, I would just research. And I’d just go pretty far down the rabbit hole. Okay? And that’s actually, in 2010 was when I started to look at blood markers. And it was great that I learned from people like Daine McDonald actually. James Lovell as well. Looked at a lot of stuff that Chris Kresser … so, you know, Sarah Godfrey when it actually came to female hormones and so forth.
So I started to go further and further down the rabbit hole when it came to how the body worked and so forth. And it was at that point, when I started to look at blood markers and so forth, I started to realize there was a lot more to it than just the function and the structure of that particular blood compound and so forth. And actually, a lot of the things that I’ve adopted now, when I look at your blood markers, I’m looking at how do you assimilate food. Okay? How do you break down protein? How do you break down things like lipids? How do you break down things like carbohydrates? And actually, your blood compounds can be a good indication of bacterial byproducts and so forth that you might actually have in your body. Yeah, okay?
Because you understand, when people look at things like blood markers and that most of the time they’re looking at just the function and what that actually particular blood compound does. Does that make sense? And for me, it’s the correlations that are the most important. Okay? So how does that blood marker correlate with this blood marker? And what it actually represents. So I can look at someone’s blood markers, which wasn’t taught to me. Was actually came about from me comparing blood markers to stool analysis and actually seeing that there was trends in your bloods that were indicative of issues like SIBO, like small intestinal bacterial overgrowth. Actually having high antibody response, which was an indication of things like intestinal permeability. And …
So just on that, what are some of the blood markers that you see indicative of that? [crosstalk 00:07:17]
Yeah, okay.
If a practitioner’s watching.
I mean, there’s obviously a lot of trends that I see in blood markers and so forth, but if I just use a few indications. One would be the MEBs, with is the monocytes, the eosinophils, and the basophils. Yeah, okay? And in layman’s terms, the eosinophils and the basophils, bless you. Yeah? The eosinophils and the basophils they’re like pro-inflammatory white blood cells so they can be actually a sign there’s high antibody response taking place. Which basically means that there’s things going into the blood stream that are causing a histamine reaction and a antibody response and your body has to also produce antiinflammatory mediators and so forth to respond to that antibody response taking place. Yeah, okay? And if the MEBs are above 0.7, like they’re 0.8 or above, that means potentially there could be a lot of histamine reaction, a lot of antibody response taking place. Which could be the initial signs of something like intestinal permeability or some sort of structural damage to the epithelium or the mucosal lining.
So that’s one indication, but something like SIBO, for instance, I’ll just probably use a couple of examples. But something like SIBO, something like your total bilirubin …
Just before you can get to SIBO, just so it’s a complete podcast, what is SIBO?
SIBO is small intestinal bacterial overgrowth. That’s what it basically stands for. Now, if you’re going to ask my opinion, they basically say about 60% of the population have IBS. Not a 100% sure where they’re pulling that statistic from, yeah, okay? But I think something like IBS, which is irritable bowel syndrome, okay, for me I think it’s a bit of a medical sort of terminology. Yeah, okay? Because, okay, you’ve got an irritable bowel. But why do you have an irritable bowel, okay? It’s not actually giving me answers to what’s actually going wrong internally in my gastrointestinal tract. Yeah, okay? So we could say you’re responding quite badly to particular types of foods. Then you eliminate those foods. Yeah, okay? But does that solve your problem? Okay? That’s just food avoidance. Yeah, okay?
And you understand that most people are going through this food avoidance thing. Where they’re going, “Well I react pretty bad to zucchini.” Or, “I react pretty bad to chicken.” And so forth. So then they avoid those foods. Yeah, okay? And I’ll get into this a little bit more later, but your food sensitivities change every three to four months. People need to know that. It’s actually based on food rotation and so forth. Yeah, okay? And something like, really what IBS is for me is really SIBO, okay? And so we could say that maybe up to 60% of the population have something like SIBO. Basically you’ve got bacterial overgrowth in the small intestine. Okay?
Because most of your microbiome should be located in basically which area of your gastrointestinal tract? Most of it should be located in your large intestine. You have about 400 different species in the large intestine. Yeah, okay? And it’s not that you don’t have species in the small intestine but most of the time the species that we see in the small intestine are things like lactobacillus mainly. Okay? And also small amounts of like bifidobacterium and so forth. But most of your microbiome should be in the large intestine. You’ve got things helicobacter in the stomach and then you’ve got about 40 different species in the mouth.
But basically what’s happened with people with SIBO, a lot of people, a lot of the literature you’re going to read, people are going to say, “Oh, it’s caused by heavy metal toxicity or hydrochloric acid issues.” Because basically, if you’ve got hydrochloric acid issues you’re not breaking down the food efficiently which means it sort of gets passed down into the small intestine. Where basically the small intestine goes, “What the hell’s going on here?” Yeah, okay? Because now the small intestine’s got to work a lot harder to break down the macronutrients which means it sits there and ferments for longer periods of time. Which is going to encourage bacterial issues.
But more for me, something like SIBO is actually caused by like epithelium damage. And so what I mean by that is more likely mucosal lining damage. Okay? And there’s all this different types of damage that you can actually cause to the microvilli and the sub mucosa and actually the villi itself. And it might get into this [inaudible 00:11:31] and that can cause a whole array of different symptoms. Yeah, okay? Now, if I’m struggling, if I’ve got issues with the brush borders and the microvilli and I’m struggling to break down the macromolecules and the micronutrients and all that type of stuff, that’s going to affect transit time. Does that make sense? Which means a lot of these food particles and that, they’re going to sit there and they’re going to ferment for longer periods of time. Okay?
So if they’re sitting there and they’re not getting broken down properly, then that’s going to encourage bacteria to travel from the colon, up the ileocaecal valve into the small intestine where they’re essentially going to do what? They’re going to sit there and they’re going to feed on the food that is fermenting. Does that make sense? And most of the time, we don’t really know what the full break down of the microbiome is, when it comes to SIBO, but it does tend to be E. coli. Okay? It tends to be E. coli, clostridia which is clostridium, okay? And bacteroids. Yeah, okay? So they tend to be the major bacteria.
What are bacteroids?
Yeah, they’re just another form of microbiome. Yeah, okay? And I want to understand is, sometimes it can actually be an overgrowth of bacteria that you do actually require. Does that make sense? So yes, it can be bacteria that is pathogenic in nature. Okay? And most of the time with SIBO it tends to be bacteria that is pathogenic in nature. But it can just be an overgrowth sometimes of good bacteria as well. Because I don’t want to demonize a lot of the microbiome, okay? Because even the bad stuff, to a certain extent. Because it’s a little bit like happy families in there. Okay? So you should have a bit of a balance between the good bacteria and the bad bacteria. Yeah, okay?
And most of the time, our issues are ratio issues when it comes to the microbiome. Yeah, okay? So does that sort of make sense with SIBO? [crosstalk 00:13:14]
Yeah.
So you’ve actually got an overgrowth of bacteria in the small intestine. And this is where, obviously the fermentation rate of certain foods becomes problematic. Yeah, okay? Because if you look at things like carbohydrates, okay? So one quart, which basically means one particle of carbohydrates equals 10 quarts of hydrogen ions. Okay? So you’re producing excess amounts of hydrogen ions in that scenario because that stuff, the carbohydrates, is sitting there and it’s fermenting for longer. Which encourages more hydrogen ions. And actually, too excess amounts of hydrogen ions in the small intestine can actually cause issues with what we call T-R-P-V-1 receptors. Which actually, in layman’s terms, causes bacillary relaxation. Okay? And that’s why a lot of people when they’ve got something like SIBO, they get things like diarrhea and so forth. Yeah, okay?
And then because you’ve got the excess amounts of hydrogen ions, in the system, you’ve got a particular bacteria called archae. And the role of archae is to break down the excess amounts of hydrogen ions. Okay? But what is the byproduct of archae? Methane. Okay? So now, all of a sudden, you’ve got excess amounts of methane in the system as well. And that’s why people will belch and flatulence and they will get that generally after high amounts of carbohydrates because they’re sitting there and they’re fermenting for longer. Does that make sense? Yeah, okay?
And so people naturally might go-and that’s why a lot of FODMAP map has really come into the fore, because low FODMAP is based on foods that don’t sit there and ferment for long periods of time. Does that make sense? And a lot of people go, “Well I just feel amazing on a low FODMAP diet. And I’m going to stay on a low FODMAP diet for the rest of my life.” Yeah, okay? And that’s one of the worst things you can do because actually, high FODMAP foods are exceptionally good for you. Now why? Because they provide food for the microbiome and so forth. And they’ve got their own nutritional benefits. And actually, a lot of those high FODMAP foods, especially things like garlic and onion and so forth, they got properties like inulin that are actually, essentially, food for the epithelium. They’re actually food for the mucosal cells. Does that make sense? They actually help with the structure of the mucosal cell. And help with things like secretory IgA.
So, question about the FODMAP diet, right? Say I’m on low FODMAP, I’ve cut out all these foods. We’re calming down the reaction in the gut. When can we start adding in the carbohydrates?
Yeah, it’s a great question because it just depends on, obviously, what the issues are that are actually going on in the gastrointestinal tract. Because those issues can be quite diverse and it’s going to differ from person to person. Yeah? So for instance, if, obviously, in this … like, when we’re talking about SIBO? Yeah, okay? Because SIBO would be a justification for going on something like a low FODMAP regime. But just people need to understand that if you’ve got something like SIBO, it’s very very likely also that you’ve got mucosal lining damage. And that’s actually why you’ve got the SIBO in the first place. Okay?
Now is there a lot of research to back up that fact? Not necessarily. Yeah, okay?
So it’s a Dave special.
It is a little bit. Yeah, okay? Because I think what you’re going to find is that more and more research is actually going to point that if you’ve got mucosal lining damage, and potentially things like intestinal permeability … I don’t like to say intestinal permeability or leaky gut all the time, because I’m just basically saying that people have got damage to the gut lining. Okay? And that, the type of damage that you can have to the gut lining is quite diverse. Does that make sense?
Why would they have damage to the gut lining?
Yeah. There can be numerous factors that would contribute to that. Yeah, okay? Because … it’s a good question, yeah? Because everyone, when they sit in my office, they go, “What caused this?” And they want to know the one thing that essentially caused it. [crosstalk 00:16:59]
Gluten!
Yeah. We’ll get to that in a minute, yeah?
Just blame the gluten for everything. It works.
Yeah. And well, for a long time people would just blame gluten or gliadin. Okay? Because essentially, it stimulates a particular tight junction protein, which is called zonulin, okay? And even if you look at the research, because this came about from a research paper from a guy called S. Drago, okay? In 2005.
Guy from Rocky, right?
Well I don’t …
If he lives, he lives. If he dies, he dies.
That’s pretty impressive. Very smart as well, yeah, okay? But basically, this research paper which is sort of … I backed a lot of the things that I used to say on this research paper as well. I don’t necessarily think that he was trying to claim that gliadin or gluten was a necessarily really bad thing. He was just talking about the reaction that happened in the gastrointestinal tract. And he actually proved that the gliadin molecules stimulated zonulin. And basically, because that’s the gatekeeper to the tight junctions. Yeah, okay? And basically, what would happen is that would tell zonulin to open the junctions a little bit wider, okay? Which means you’ve got hyper-permeability through the tight junctions. Which means certain enzymes and protein molecules would be getting through those tight junctions into the hepatic portal system. So blood stream, liver. And causing like an antibody response. If you’ve got an antibody response, there’s going to be cellular activation. So you’re going to stimulate white blood cells and then guess what? Then your body’s going to produce antiinflammatory mediators like prostaglandins and all these things.
You can tax those things because they’re essentially dependent on things like Omega-3s and all this type of stuff. And that’s why you can tax your stores of Omega-3s, if you’ve got a lot of antibody response and a lot of inflammation taking place. Does that make sense? So he wasn’t necessarily, I think, trying to say that this is really bad. He was just saying that this reaction takes place whether you’re Celiac or non-Celiac. Okay?
Now, in a healthy gut environment, okay? Things like calcium … so minerals would actually go up the tight junctions. Yeah, okay? And that actually would tell zonulin, because it’s like the zipper. So calcium’s like the zipper, where it tells zonulin to pull the junction tight again. Yeah, okay? But when I am in an unhealthy gut where I’ve actually got damage to the sub mucosa and actually the epithelium and the mucosal cell, well then the problem is you can have our issues with micellizing factor. Which means you struggle with fats and oils. Which means a lot of the calcium can get stuck in the fat deposits, the things that are not getting broken down properly. Which means the calcium isn’t really going up the tight junction. Which means it’s not telling zonulin to tighten that junction again. Okay?
So in an unhealthy gut environment where someone has worn down the gut lining, then gliadin becomes a problematic thing. Because more, for me, it’s an exacerbator. Does that make sense? I don’t think it’s the devil. Far from it. But back in the day, I just used to say to people, “Gliadin’s the devil. Yeah, okay? And that’s basically what’s causing your intestinal permeability.: And the likelihood is, it’s not really.
So what is?
Most of the time it’s things like chronic stress. Because if you would just look at the stress response, now we need to understand if when I am having a stress response that initial stress response starts in your hypothalamus and you produce a thing called corticotropin releasing hormone. And corticotropin releasing hormone in high amounts, tells your digestive systems, because it down regulates ghrelin. And ghrelin’s your hunger hormone. Yeah, okay? So all of a sudden, because you don’t want to be trying to digest food in that stressed state. Does that make sense?
And then that, because it just … need to understand about digestion and breaking down food. Don’t get me wrong, because obviously I’m talking about it. Yeah, okay? It’s important, but is it imperative? Okay? In moment and time, is it imperative? Yeah, okay? And I would argue, in moment and time, there’s three functions that are imperative for the body to deal with because it just comes down to survival. Okay? And the whole thing is, stress response in moment in time, okay? Is imperative. Because if I don’t respond to whatever that … so if it was a guy coming, charging at me with a knife? And say I’m sitting here eating my sardine salad, because I’d probably eat sardines. Yeah, okay?
Canned sardines, or?
Yeah, canned sardines all right. I’m not going to go into the … whatever the can’s being made out of and the heavy metal toxicity. [crosstalk 00:21:18]
Oh, come on Dave.
But generally, sardines are a little bit of a cleaner fish.
You’d be eating fresh sardines? Or are you getting canned?
Fresh sardines would be better, for sure. Yeah, okay? But I’m sitting here, eating my sardine salad. This guy comes charging at me with a knife. Now, what’s more important: me digesting the sardine salad or me dealing with the guy with the knife? Yeah, okay? Now, I’ve got to deal with that stress response. And you can understand, people have got this stress response going on constantly throughout the day and your body does not understand the difference between maybe this instance of the guy coming and charging at you with a knife and your boss hassling you, yeah, okay? Or you’ve got problems, emotional stress at home. Does that make sense?
It’s still a stress response in the body. Which means you’re going to have this reaction. Yeah, okay? So that’s the body needs to respond to that because the body perceives what could the end result be. Death. Yeah, okay? And the other one, if I’m having a stress response, are you going to elevate blood glucose levels? Yes. Because you’ve got to have energy to deal with the situation. Does that make sense? Okay? So blood sugar would be another imperative function in moment and time, okay? Because if you don’t stabilize your blood sugar levels or you don’t elevate your blood glucose to deal with that situation, yeah, okay? And you don’t stabilize your blood sugar levels, potentially you could slip into a coma, okay? And you could die, okay? So once again, the body’s going to prioritize that situation.
And the third one, which I think is a little bit of the overlooked one, is antibody response. [crosstalk 00:22:45]
Okay.
Yeah, okay? And that’s actually to do with bacteria. Yeah, okay? Because if I don’t deal with bacteria, okay? What could the end result be? Well that bacteria can start to attack my cells. Yeah, okay? And if it’s attacking my cells, what could the end result be? It could be disease, illness, and eventually … [crosstalk 00:23:02]
So how is the body dealing with bacteria?
In terms of what’s it throwing at it to deal with it?
Yeah. [crosstalk 00:23:08]
Yeah. Well it’s going to produce antiinflammatory mediators, yeah, okay? Even your good microbiome, they actually produce antibodies that help you fight bacteria that’s attacking your cells. So there’s many mechanisms that they use to enable you to fight bacteria that’s potentially attacking your cells and so forth. But also, micronutrients, yeah, okay? Because your white blood cells and so forth. And what we’ve got to understand with white blood cells, I always say this to people, yeah, okay? That you don’t have a Oompa Loompa factory in your body. Okay? So there’s not guys spinning away at their wheels and producing more, an infinite supply of white blood cells. Yeah, okay?
Because you look at things like white blood cells, they come from stem cells within your bone marrow. Okay? But what’s one of the key building blocks for stem cells? Vitamin A. Okay? And what do I actually need, it comes down to micronutrients for me. Yeah, okay? And if we look at vitamin A, that’s …[crosstalk 00:24:03]
So like unlocking the waterfall.
Yes. TLC.
Yeah. Yeah.
Yeah.
Yeah.
Oh, the same, basically. Yeah. Vitamin A is one of the key micronutrients that we actually need for the stem cells. And then if I actually look at other micronutrients that they need, something like vitamin C. Vitamin C actually helps with your ability to synthesize white blood cells. Yeah, okay? You look at vitamin D. Now vitamin D for me, it’s sort of like the backup. Yeah, okay? Because when you convert vitamin D into its more bio-available form, more bio-active form which is 125D. That actually allows you to produce antimicrobial peptides that actually fight bacteria. That’s why vitamin D is essential for clearing bacteria and so forth.
But imagine my vitamin D stores are really low, okay? Then that puts a lot of pressure on my white blood cells now. Does that make sense?
So, in other words, just to recap on that: you’ve got vitamin A, vitamin C is the forefront, frontline in this …[crosstalk 00:24:59]
And there’s other micronutrients as well.
And then you have vitamin D, which you’re referring to as the backup. So it’s when you see low vitamin D that’s highly concerning?
Yeah, because that can actually be a sign that the body’s having to produce a lot of antimicrobial peptides to potentially fight bacteria that overgrowth of bacteria in the gut lining or in the body. Does that make sense? Yeah, okay? And also, you look at things like neutrophils, yeah, okay? And neutrophils are really interesting in blood markers. Because they do tend to be extremely low most of the time. Yeah, okay? Which is a sign of immunosuppression. And neutrophils are like … they make up about 50% of your white blood cell supply. And their real role, because they’re part of your innate immune system which means like initial responders. But when I say initial responders, they take about six hours to get to point of infection. Yeah, okay?
But neutrophils are the heavy hitters against things like negative gram bacteria, yeast, mold, mold spores, candida, all these types of things.
You’re just opening up so many topics. I do want to get back to one thing that we went before, and we’ve kind of danced around a little bit. Why is it damaged? And I have heard something around the gut, that the gut lining can repair itself every five days.
Yeah.
So why, say I go on a FODMAPs diet for five days. Why isn’t my gut rebuilt, number one. Why can’t just removing the offending foods start the process of rebuilding? But why is it the wall, the epithelial wall, damaged in the first place?
Because more, for me, it comes down to the allostatic load on the gut for most people is huge. And what I mean by that, remember I said there’s not generally one factor that is causing this deterioration. It tends to be a multitude of different factors. Yeah, okay? [crosstalk 00:26:39]
So people are too stressed?
Yeah. It can be things like emotional stress. Yeah, okay? So we can actually know that people, and it’s actually proven through medical research, that when people have more things like emotions like fear and anger and sadness and so forth, that we know that these emotions start to wear down the mucosal lining. Now, in particular, they’ll actually affect your secretory IgA levels. Okay? And if we actually look at a secretory IgA, which is an immunoglobulin which means it’s a protein molecule, okay? Which is really, really abundant in mucus. Okay? And so we’ve obviously got mucus when it comes to things like snot and tears and saliva. But actually one of the highest amounts of mucus in the body is in the gastrointestinal tract. Yeah, okay?
And secretory IgA, I like to use the analogy of it being a little bit like a Venus flytrap. Okay? So it’s actually produced within the epithelium, within the mucosal cell. And that rises more to the surface, like the apical part of the cell. Or the brush borders, yeah, okay? And there it’s sort of is like a Venus flytrap. It’s like a sticky substance and it traps in pathogens and microorganisms and so forth. But we actually know that when you’ve got a lot of emotional stress and it’s actually some of the smartest brains that I think going around like Bruce Lipton and Gregg Braden they’ve actually done research to show that your emotional state will actually wear down the secretory IgA levels.
Now when I do things like stool analysis and so forth, because the highest concentration of secretory IgA is in the gut lining, well it’s going to come out more in things like your stool. Okay? And so sometimes, if you’re producing a lot of it because you’re going through a high emotional state and so forth, then there can be a high amount of secretory IgA in your stool. Okay? So it is quite a sensitive market, you’ve got to take it with a pinch of salt. But then over time, what do you think is going to happen to your secretory IgA levels? Okay?
If you’re not fixing things like the emotional state that you’re in and so forth, then your secretory IgA levels over time, they’re going to drop down. Okay? A lot of people, when I look at their stool tests, one of the most common scenarios I see is that the secretory IgA level’s extremely low. Okay? And when the secretory IgA level’s-and I don’t just use one marker, I just need people to understand. I’m not just basing that people have intestinal permeability and damage to the mucosal lining based on one marker, because I’ll correlate it with other markers within the stool that can actually be a representation of something like intestinal permeability as well. Yeah, okay?
Well this is a great time just to say, this is not health advice. Health disclaimer: this is not health advice. Do seek medical advice. This is only for entertainment purposes only. This is not … do not take what Dave’s saying and then apply it to yourself and go, “All right. I had that thing that you said and I just went on the FODMAPs diet.” And yeah, so don’t be that guy. Don’t be that girl. This is not health advice. Entertainment purposes only. Anyway, continue.
Hundred percent, yeah. I agree.
Yeah, so in that instance, yeah okay, like someone’s negative emotions and so forth? That can be one factor that actually starts to deteriorate …
What other factors? So you’ve outlined that stress is a big thing, right? And emotional … so I’m just trying to get through my head because … well, firstly let’s start with a premise. Is it true that you can heal, like the gut rebuilds every five days? You have a new gut lining every five-in a healthy person? That was sort of one of the axioms in the Poliquin days.
Yeah. The whole thing is, most of the time people’s gut lining is so deteriorated because once again, you can actually get damage to so many different areas within that, within the gut lining.
I suppose … [crosstalk 00:30:15]
You might get deterioration of the actual villi, okay? So you can have deterioration of the microvilli, you can actually cause damage to the sub mucosa. You can actually cause damage to the villi. Yeah, okay? So we’re talking about the bigger structure within the small intestine. And actually, when you start to get damage to the actually villi itself, yeah okay? Which they call crypt hyperplasia. Yeah, okay? That’s actually … those people start to get problems with amino acids. [crosstalk 00:30:42]
Right. That’s …
And when they start to get problems with things like amino acids well what do you think that’s going to start to affect? [crosstalk 00:30:47]
Recovery.
But also neurotransmitter balance.
Yeah.
Okay? Because we’ve got to understand, particular byproducts like neurotransmitters and hormones, yeah okay?
Schizophrenia could start [crosstalk 00:30:58]
Well they’re essentially derivatives from food. Does that make sense? But if I’m not actually breaking down the singular amino acids properly because I’ve got issues within the villi and so forth, that’s going to affect things like my neurotransmitter balance. And it’s also going to affect things like my hormonal balance. Because you look at neurotransmitters, they’re essentially biogenic. Which means basically the precursor is an amino acid. Okay? So altriptophan gets converted into serotonin. Yeah, okay?
And you’ve obviously got things like phenylalanine gets converted to tyrosine and then into dopamine. Yeah, okay? But if I’m not able to assimilate these amino acids properly, that’s going to affect my neurotransmitter balance. So if I’ve got villi-atrophy, yeah, okay? All of a sudden you start to get neurotransmitter and hormonal issues. Does that make sense?
It does. So if I … I’m trying to paint out this picture in my head where to stack the deck, say someone comes in and they’re all, “I need to recover my gut in the fastest time possible.” They go on the FODMAPs diet, because it does come back to the question of when can people reintroduce these foods from the FODMAPs diet. So they’re on the FODMAPs diet, let’s say they go to a Club Med for let’s say a week. They’re on holiday. There’s no stress. They’re all that good. Is that warrant? What else affects the recover or the time in which they can bring back those carbohydrates?
Yeah, once again it does depend on the individual. I know I’m not necessarily giving a straight answer on this. Because if certain cells within the gastrointestinal tract are in a good state, then that actually allows you to heal particular epithelium. So other mucosal cells. Because people need to understand there’s many different mucosal cells in the gastrointestinal tract. Okay?
So it’s not a case that there’s just one type of mucosal cell that you’re damaging. You’re generally damaging all these different types of mucosal cells. Which I can go into a little bit more. But some of those cells they actually help to heal the other mucosal cells. And one of them is called progenitor cells. Yeah, okay? And so progenitor cells, if we’ve actually got the, once again the villi, they actually sit more towards the base of what we call the intestinal crypt. Yeah, okay? And the role of the progenitor cells is … they’re actually to do with neural stem cells, okay? So these are the ones that actually, are related to the enteric nervous system. Which is the communication between your gut and your brain. Okay?
So we’ve got a nervous system that exists between our gut and our brain. And I think a lot of the time, we’ve damaged that communication between the gut and that brain. And these progenitor cells … [crosstalk 00:33:31]
How have we damaged that?
Yeah. Well, once again, it’s just that it’s a combination of how we’re handling emotional stress. Okay? So that’s one factor.
So is the forefront of recover for you, a lot of the time, emotional health?
Yes. Because even like when I probably talk about some of the things you can do to start to repair the gut lining and so forth. So I’m going to be honest. It’s quite easy for me to make inroads into repairing the gut lining. Okay? I think if someone’s caused severe damage over a long period of time, it may take you about two to two and a half years to fully repair that. Okay? Now that flies in the face of what they’re saying where we could potentially repair it within five days and so forth. Because sometimes the damage is so extensive in the mucosal lining, it’s going to take awhile, yeah? To actually make bigger inroads into it. Yeah, okay?
And I’ve seen that in so many different people. And actually, I saw it in myself. Okay? I had such bad intestinal permeability. Literally, I was urinating out my backside about six times a day. I started to have serious neurological problems. Okay?
It’s like you’ve read my notes. Because that was the next place I wanted to go. Exactly that. Eh, tell me about the times when you urinated out of your backside? Eh? You saw my notes on that? What?
It goes back to the waterfall, doesn’t it?
It does, eh?
TLC. Yeah.
Don’t be chasing those scrubs.
Yeah. And so, the reason I went so far down this rabbit hole with the gastrointestinal tract is because I lived that nightmare.
When was that for you?
So basically, it really probably came about … that’s pushing my brain a little bit. But probably when I came back from London, strangely enough. Yeah, okay? Because obviously when I was in London, look, I pushed the envelope. I partied pretty hard. Yeah, okay. I drank a lot. Yes, of course I on the outside I might have looked fantastic. Yeah, okay? I had a six pack and I trained pretty hard, but I was pushing the envelope. Like I would train maybe 10 to 12 people in a day. I was doing up to 55, 60 hours plus in a week. And then on the weekends, I’d go out and I’d party really hard. Okay?
And yes, I was actually eating pretty clean back then. Yeah, okay? But I pushed my body to the brink. Okay? And then that was coming at a detrimental harm down the line, to my gut. And actually, how it manifested for me initially was energy system issues. I started to get really lethargic. Really tired. Okay? And actually it wasn’t until quite further down the line that I actually started to get a lot of gastrointestinal problems. Yeah, okay? And before that, my brain started to break down on me. Okay?
So I actually went from an extremely social person to actually having extreme social phobias. So I couldn’t stand being in a social setting. And that was the complete opposite of actually what I was like. Yeah, okay? And actually, I had even like a photo phobia. Okay?
So this is circa around 2010, 2011?
Yeah. 2010, 2011. Probably 2012 as well. Yeah, okay? And I even was scared of getting my photo taken. And believe it or not, having photo phobia and actually a scare of things like flashing lights and getting your photo taken is actually linked to a particular strain of bacteria. It’s actually linked to alpha-hemolytic streptococcus. Yeah, okay?
Now, it’s strange enough. When I actually did stool testing further down the line, what do you actually think I had?
That bacteria.
Yeah. I actually I had an overgrowth. Now in very, very small amounts that bacteria is not pathogenic in nature. It can actually cause things like strep throat. Yeah, okay? And even things like sepsis and toxic shock syndrome and infection in the red blood cells and so forth. It is linked to neurological problems like phobias and so forth.
Do we get sick because of the emotional component? Or are we getting sick because of the physical component? Which one, in your opinion, body and mind which one? Is it the chicken or the egg?
I think the best way to explain where I’m coming from, yeah, okay? Is that I … because I’m putting a lot of emphasis on the gut, correct? Okay? But I actually don’t think it’s where a lot of people’s problems start. Okay? I actually think most people’s problems start in the brain. Okay? So it’s actually emotional stress. Yeah, okay. It might be things like social conditioning. Yeah, okay. Might be their belief systems, yeah okay. Their insecurities. So a lot of these things, these negative emotions and so forth. But you understand then there’s other stress loads. Okay? So exposure to things like chemicals and heavy metals. Yeah, okay?
So then we’re putting into our body things like food additives and colorings. Yeah, okay? So they start to exacerbate it. Then, when you’re dealing with something like gliadin or gluten. Yeah, okay? The concentration of gliadin is a problematic thing. Because now it’s a higher concentration. Which means now it’s also making more hyper-permeability in the tight junctions. Does that make sense? Okay?
So that’s exacerbating it. Yeah, okay? And then it can be our water. Because our water essential … I know, water is pretty much involved in every single biological function in the body. And the structure of that water is really, really important. It contains things like … unfortunately, things like chlorine. And guess what it doesn’t have? It doesn’t’ have a lot of the minerals and the microminerals that it should contain. Yeah, okay? Things like magnesium and chloride tends to be all right. But this sodium concentration is not as good. Yeah, okay?
So we’re drinking … the water structure has chemicals and they, in small amounts start to deteriorate the gut lining and so forth. Does that make sense? And what people need to understand is, if I’m starting to have a lot of these antibody responses and so forth, well guess what? Your own immune system can start to deteriorate your gut lining. Yeah, okay? Because even like, if I start having high neutrophil activity because I’ve got the antibody response, well neutrophils are what to do with H2 receptors. Yeah, okay? Which is histamine receptors. Okay? So they actually start to ’cause aggravation in the gut.
And then guess what? Now you’ start to get bacterial issues. And the by products of bacteria, so things like LPS, like lipopolysaccharides, yeah, okay? And acetaldehyde which you get … [crosstalk 00:39:36]
Let’s go back to that. What are lipopolysaccharides?
So lipopolysaccharides are like fatty acid molecules and long chain carbohydrate molecules. Like monosaccharides and polysaccharides, okay? And LPS is basically, it makes up the outer membrane of negative gram bacteria. Okay? Now I need people to understand, is that negative gram bacteria is not the devil. Okay? Going to draw some pictures, eh?
[crosstalk 00:39:59]
Yeah, okay. Yeah. Yeah. So negative gram bacteria, I just wanted to really emphasize this: is not the devil. Okay? Because we’ve got pathogenic strains of negative gram bacteria but we’ve also got non-pathogenic strains of negative gram bacteria. Does that make sense? Yeah, okay? But when you’ve got an overgrowth of the pathogenic strains of negative gram bacteria what can actually happen … because once again, it’s a ratio issue, okay? Which means when the bacteria, which is an endotoxin, when it’s actually getting broken down what it will actually do is expel-which I’m going to draw in a minute-it’s going to expel more LPS into your system. And the LPS can actually cause more damage to the epithelium and the mucosal lining. Yeah, okay?
Now, the important thing to understand as well, okay? When there’s more LPS in things like your blood stream and so forth, yeah, okay? Then unique things like glutathione which is the master antioxidant, yeah, okay? That’s actually required to clear a lot of these byproducts and so forth out of the system. So essentially, excessive amounts of LPS it actually cannibalizes glutathione. So your glutathione pools tend to be on the lower side. Yeah, okay? And glutathione is synthesized in the liver. Yeah, okay? But then glutathione deals with some of the most stubborn xenobiotics. Yeah, okay? So it deals with things like heavy metals and plastics.
Now, if I play devil’s advocate here, okay? Because my glutathione pools are depleted because I’ve got excessive amounts of LPS which is coming from the negative gram bacteria, now I’m going to be exposed to heavy metals whether we like it or not. I don’t want it to be doom or gloom, but we are going to be exposed to heavy metals in a modern society.
And we’re not talking about AC/DC either.
No. Far from it, yeah?
Yeah, so we are going to be exposed to these things, yeah? Now if I’m accumulating more heavy metals, I need the glutathione, yeah, okay? And I need the sulfation pathway with is another liver detoxification pathway which tends to be down when you’ve got things like SIBO and intestinal permeability. So the problem is, is that because I don’t have the glutathione pools, then the heavy metals start to accumulate. Okay? So all of a sudden I’ve got more heavy metals in the bloodstream. And guess what? More heavy metals in the bloodstream and things like mercury and so forth, they can start to lodge in certain areas of the body. And especially areas like the brain. And that will affect things like the nigra and the nigra is where I produce more dopamine. Yeah, okay?
And so it starts to cause a negative effect on dopamine. But it’s also can affect things like acetylcholine. Yeah, okay? And if I’ve got issues with … I’m just playing, I’m just letting people understand the cascade effect in the body. And if it’s impacting things like acetylcholine, okay? And acetylcholine is the gateway to the vagus nerve. And the vagus nerve helps with communication of the brain to the heart. Yeah, okay? But it’s also part of the enteric nervous system. It’s all interconnected. Enteric nervous system is to do with the gut and the brain. Yeah, okay? Then the vagus nerve is the key to the parasympathetic nervous system. So what is that going to effect? That’s actually going to affect rest and digest. Does that make sense?
So you can get someone who has gastrointestinal issues. Let’s take two people. Put them in an environment where they’re exposed to toxins and heavy metals. One person’s got gastrointestinal issues. And the other person doesn’t. I’m telling you the person who’s got gastrointestinal issues, they’re the one that’s going to have problems with heavy metal toxicity and so forth. Because they don’t have the compounds to be able to clear the excess amounts of heavy metals out of their system. Now we just generally say, oh, that guy is unlucky. Okay? I’m just saying it’s probably down to the fact that that person had gastrointestinal issues. Does that make sense? Okay?
And for me, once we actually start to fix the structure of the gut and we actually start to realign [crosstalk 00:43:53]
So …
The natural microbiome …[crosstalk 00:43:54]
Then why does that guy have the gastrointestinal issues? Is that simply because what, in your experience that guy stresses more than the others? Or thinks more, has more emotional load?
It’s just an exacerbation of many, many different factors. You’ve actually listened to people that would say contribute to things like intestinal permeability, you can have up to 18 trigger factors for something like intestinal permeability. And they generally say if you have five or more of those trigger factors, and a lot of the things are things that I’m talking about. Okay? So it’s the [crosstalk 00:44:23]
Stress.
The byproducts of bacteria. Yeah, okay? Things like nitric oxide. People need to understand there’s different forms of nitric oxide, yeah, okay? You’ve got inducible nitric oxide which is what your body produces when you’ve got bacterial issues. But that can cause issues and deterioration of the mucosal lining and the gut lining. Yeah, okay? The LPS that I was talking about. The acetaldehyde which is a byproduct from things like parasites. And yeast and candida. They can also contribute to deteriorating this gut lining even more. Because the acetaldehyde essentially, what it does is actually shrinks the epithelium. So it actually makes it essentially smaller. Which means you’re losing surface area in your gut. Does that make sense? Okay?
So those are factors. But also your own immune system might produce [inaudible 00:45:07] more things like basophils. Having too high a histamine activity, because remember I said when we have this stress response, yeah, okay? We also, because histamine is also going to be released, yeah, when we have a stress response. Yeah, okay? And so if we’re releasing more histamine, I don’t want people to think of histamine as the devil. Yeah, okay? Because histamine as a neurotransmitter actually helps with sleep/wake cycle, it actually helps with regulation of things like libido and so forth. And as a hormone, it actually helps to make our gut more permeable.
Now a lot of people are going to go, “That’s bad.” But it does that for a reason: so it can transport things like platelets and red blood cells and white blood cells around the body so that we can respond to the antibody response. Does that make sense? But what happens, all of a sudden upon producing too high amounts of histamine, does that make sense? And one of the by products of something like SIBO is excess amounts of histamine. So now I’m making my gut even more permeable. Does that make sense? Yeah, okay? So even histamine can contribute to that load on the gastrointestinal tract.
And once again, we just talked about the emotional stress. We talk about the pollutants and the chemicals. And so for me, there’s … I can’t give people the one thing that is actually causing a lot of the gastrointestinal stress. Because you know what? For me, it’s a multitude of these things. It’s the exacerbation of all these things that is actually making the deterioration of the gut lining more significant than ever before.
So what you’re saying, Dave, is if I drink kombucha every day everything will be fine. But what about gutright? I take that gutright supplement and then everything will be fine as well.
Yeah. And that’s why if you flick through the comments, yeah okay, you’re going to get a lot of people who are saying, “I don’t feel too good on this.” Yeah, okay? Because if you look at a gutright supplement … I’m not here to bad mouth supplements and so forth, but just when it comes to the gut you need to understand more evidence. Okay? Putting these things in, you could … so one person’s medicine is another person’s poison.
So what’s your stance on kombucha?
Well …
Because I know there’s people watching it going, “Let me just fix this with kombucha. Let me go and [inaudible 00:47:19] island on Club Med and just take some kombucha and …” You know.
And that’s the thing. Look, in a healthy gut environment, having a little bit of kombucha now and then is fine.
What’s now and then? Twice a week?
Look, having it maybe once a week. I like a rotation when it comes to a lot of things that help with microbiome. Like prebiotics and so forth. So even thinks like pectin which is the skin on fruits. But that doesn’t mean that you should be sitting there eating a truckload of nectarines and peaches and apples, yeah okay? Because you only need small amounts of these things to actually help with the microbiome. Does that make sense?
Even when it comes to resistant starch. Yeah, okay? And you’ve got all these different types of resistant starch. Yeah, okay? But if I’ve got microbiome imbalances, yeah okay? You understand that these types of things they’re not partial to what they feed you. Okay? So if I’ve got a ratio issue, yeah okay? It’s just going to feed whatever’s down there. If I’m drinking things like kombucha, I’m having high amounts of resistant starch, okay? These things don’t go down into your digestive system and go, “Hey, guess what guys? I’m only here to feed the good stuff.”
Right.
Okay? It’s just going to feed whatever’s in there. Does that make sense? And if it’s feeding, essentially, whatever’s in there, okay? The problem is, that’s going to cause an inflammatory response. Because unlike if it’s feeding the good bacteria, okay? Which means that good bacteria’s producing amazing byproducts like short chain fatty acids and that would be things like butyrates and propionate and acetate and then these things help with reducing inflammation and producing T regulatory cells that help your body recognize your own immune system. So all these amazing things.
When it’s essentially, when you’ve got a ratio issue where maybe it’s more like 50/50, okay? Then it’s feeding the bad bacteria. They’re not producing these byproducts. Does that make sense? And guess what? They’re releasing more of these negative byproducts that I was talking about like things like LPS and acetaldehyde and then that’s causing more inflammation in the body. Yeah, okay? And most of the time, what I’m trying to do is reduce the inflammatory load in the body. Because if I’m causing more inflammatory response and once again, it’s the inflammatory load is the issue. Because inflammation is not necessarily a negative thing. Okay? But if I’m causing high inflammatory load in the body, well understand inflammation bluntens the brush borders. So it actually causes damage to the brush borders.
Now if I’ve damaged the brush borders, and the epithelium, because they sit at the top of the mucosal cell, okay? And their job is to digest particular nutrients and things like dietary fats and so fort. But also, it’s to release enzymes that help you break down particular macromolecules and so forth. So they’re going to produce things like lactase that allows you to break down things like lactose. They’re going to produce things like maltase that allow you to break things down like maltose. They’re going to produce things like sucrase. You see where I’m going with this, yeah okay? And glucoamylase and all these enzymes that allow you to break down these macronutrients. Does that make sense?
But I have damaged those brush borders, do you think potentially that might affect how I’m breaking down these glucose molecules and so forth? 100%. Yeah, okay? And what’s going to happen to a lot of these glucose molecules and so forth, they’re going to sit there and they’re going to ferment for longer periods of time. And essentially, what could that encourage? Once again, that could encourage bacterial overgrowth because there’s a high amount of fermentation. And a lot of people when they say to me, they’ll go, “I’ve got lactose intolerance.” And even things like fructose malabsorption and and fructose maldigestion. I go, “Do you really? Do you really though?” Yeah, okay? Or is it a fact that you’ve actually got damage to the epithelium, you’ve actually got damage to the gastrointestial tract. Which means you can’t produce these enzymes allowing you to break down these particular molecules.
And I think it’s more of a sign that they’ve got damage to the epithelium and the mucosal lining. Okay? Even when it comes to things like fructose because a lot of people have a problem with fructose maldigestion and fructose malabsorption. And guess what? In the past, I’ve really demonized fructose. Yeah, okay? But understand fructose is fine. Yeah, okay? Fructose is not bad for you. It’s actually in smaller amounts, it’s good for you. Yeah, okay?
What do you define as smaller amounts?
Well once again it can depend on the person. They say if someone’s got something like insulin resistance, they might only be able to tolerate something like 25 milligrams of fructose a day. But once again, you know what? Obviously because of the fiber content in fruit … actually, fruit is really good for the gut lining. That’s the irony, yeah okay? But if the person’s got damage to the apical part of the cell, which is the brush borders, okay? So it’s the top section of the mucosal lining. I don’t know if our listeners, maybe they haven’t heard of things like the glute proteins? Yeah, okay? But the glute proteins are transporters. Okay? And so you’ve got all these different types of … they’re made up of like 500 amino acids and their job is to transport glucose compounds and substrates as well. So things like urate, like uric acid. Yeah, okay? And things like myo inositol. And so forth.
But you’ve got one particular protein called the glute five protein. And when that’s released from the cell it actually goes into the apical part of the epithelium, actually the mucosal cell. And its job, in a nutshell really, is to help with the metabolization of dietary fructose. Now, I’m just playing devil’s advocate here. Yeah, okay? But if I’ve actually damaged that mucosal lining, could that potentially affect something like the glute five protein where I can’t actually metabolize the dietary fructose properly. And I’m not saying that fructose is the issue here. And some people I have to take things like fruit away for a short period of time. Does that make sense? Because if I’m not metabolizing it properly and so forth, what type of response is it causing in the gut? It’s causing an inflammatory response. Yeah, okay? [crosstalk 00:53:30]
So it’s …
And if it’s causing an inflammatory response, that’s putting more pressure on my internal environment. Does that make sense?
So it sounds like a lot hinges on the health of the epithelium and so I suppose it comes back down to the question: what can we do today to keep that healthy? Keep that singing. Keep that as good as you can possibly get it. Because once they’re damaged, it sounds like you’re in for a bad time.
Yeah. I mean, and that’s why if, and I’ll only try and touch on this briefly, yeah, okay? But if I talk about all those different epitheliums and all those different mucosal cells, yeah, okay? Now we’ll just run through some of the major functions of what these different types of epithelium do. But the major one that actually makes up the highest proportion that line your gastrointestial tract, so your stomach and your small intestine, your large intestine is the enterocytes. Yeah, okay? And the enterocytes, actually what most people don’t realize is that 25% of detoxification takes place in the gut. So detoxification starts in the gut and guess where it finishes? Finishes in the gut. Okay?
So we’ve been putting all this pressure on the liver and saying, “Well we really need to help with liver detoxification.” I’m just going, “Don’t worry about the liver. The liver is probably the most robust organ in the body.” Yeah, okay? So we’re throwing all these liver detoxification tablets and I’m just going, “Most of the time it’s the issue upstream.’ Yeah, okay? And it can actually be damage to the enterocytes. Okay? Because the enterocytes actually allow you to produce enzymes to allow you to break down macronutrients. Yeah, okay?
And also, they all to do with antigen response. Yeah, okay? So how we’re reacting to particular food antigens and guess what? They trigger like T cells. So basically, they tell your T cells which are substrates of your lymphocytes so they’re basically immune response. Okay?
And that’s just the enterocytes. Then you’ve got things like enteroendocrine cells. And guess what? These produce hormones. Okay? So a lot of people don’t realize that within these mucosal cells that these hormones are only produced there. Okay? And so we’re producing things like glucagon-like peptide-1, okay? And glucagon-like peptide-1 which is produced in the small intestine, the large intestine-I promise I will only use this one example for the hormone. Yeah, okay? But its role is to control the emptying of the stomach into the small intestine. Yeah, okay? So if I’ve got damage to the epithelium could that potentially affect the production of this particular gut hormone? Okay? Which means the emptying of the stomach to the small intestine is quicker. Okay?
And also, glucagon-like peptide-1 helps with the release of insulin. Okay? Which basically means that the person cannot regulate their blood glucose levels. Okay? And so if I’ve got low levels of glucagon-like peptide-1 okay? Because my blood glucose levels are raising really high, okay? And then they’re going to drop really quick. Okay? So people who have got low levels of this particular hormone, they snack frequently. Okay? They just can’t stop snacking. Yeah, okay? And I know people that I’ve dealt with yeah okay, say stick to particular meals. And they’re just snacking in between meals all the time. And my argument could be, is that they’ve actually got damage to the epithelium which is actually affecting particular hormone production and so forth. Yeah, okay?
You’ve got gastric inhibitory peptides. So there’s all these particular … motilin, okay? And guess what? Motilin actually helps with gut motility. So it actually helps with how you’re churning in the gastrointestial tract. And motilin you actually produce more of when you’re fasting. Okay? So there’s all these different hormones that we’re actually producing within there. Yeah, okay?
And then you’ve got goblet cells. Yeah, okay? And these goblet cells they produce a mucus and they help to trap in pathogens and microorganisms so they protect us. You’ve got paneth cells which I already mentioned, because they produce particular enzymes like lysozymes, okay? Another thing called secretory phospholipase and they actually help us get rid of bacteria and so forth. Yeah, okay? And then we’ve got the progenitor cells. And they help with communication to the brain. But also they help with the replenishment of the other epithelium.
Now, when we damage the epithelium what I need people to understand, is there a good chance we might damage all these cells. Yeah? And if we damage … so once we actually start to damage the top of the villi, we start to damage the intestinal crypt, and then those epithelium at the base. And so that affects how we combat pathogens and microorganisms. And that’s why all of a sudden people are more prone to things like candida and yeast and parasites. Yeah, okay? So because it’s a full deterioration of that epithelium. Does that make sense?
So my argument has been, yeah, okay? Is that there’s no way that you’re just going in there and just damaging one type of cell. You’re damaging … and so the symptoms, could they be quite diverse? The different symptoms that you could get. Yeah, okay? So you could actually get neurological problems. Okay? So you’ve got neurotransmitter issues. You’ve got hormonal issues. Yeah, okay? And we know even things like your microbiome play a key role … this is, I think, the first time I caught up with you Mark I said, “For me, terrain is everything.”
Remember then we spoke about Louis Pasteur versus Béchamp and the whole, back in the 1930s I think it was, that whole thing of the paradigms and that people, the one that got popular was Louis Pasteur, the bacteria theory. That’s the reason why we have disease.
Yeah. And what I’m saying is, I like to use this, I don’t know if anyone’s seen a movie with Kevin Costner? It’s called Field of Dreams. Yeah? And there’s a particular, maybe not. It’s a older movie. I’m getting a little bit old now, yeah okay? But there’s a particular quote-it’s a baseball movie, yeah okay? And he actually builds this baseball field to basically, so that his dad can come and play. His dad’s passed away. But I’m not going to get too much into the movie, yeah okay? But basically he says this quote in it, he says, “If you build it, He will come.” And the one thing that I really want to get across to people, if you build it they will come.
And so what I mean by that is your microbiome. Okay? Because if I’m not really fixing the structure, okay? That’s not really going to encourage good diversity in the gastrointestial tract.
And I suppose, just real quick, the way you … the starting point of fixing the structure is starting off with something like a FODMAPs diet. Getting rid of the bad guys.
All we want to do, because everyone thinks, they get me rolling they think I’m anti-fruit, yeah okay? Or I’m really pro-ketogenic diet. High fat diet. To be honest, I’m not. Okay? There’s a lot of negative things that can happen if you stay on a ketogenic diet for a long period of time, okay? Because … and I’m not talking about like 85% fats here. Yeah, okay? Because that’s to get into ketosis, okay? And I want people to understand, the quickest way to get in ketosis is fast. But guess what? You’ve got to be in a pretty good state to be able to fast correctly. Yeah, okay? And actually, understand I already said that there’s huge benefits to the epithelium from fasting because you produce particular gut hormones like motilin which actually help with gut motility. So they help with that churning and they help with the churning of food and so forth. Yeah, okay?
So yeah, for me the ketogenic diet. Yeah, okay? Going 85% fats. Doing that for too long you actually stimulate particular hormones. There’s one called acylation stimulating protein. And if I’m stimulating that, that can also stimulate insulin which means the person actually starts to put on a lot of body fat. Yeah, okay? So for me, I’m talking more about 55, 60% fat. If we actually do have some damage within the epithelium and we’ve actually got …
And generally speaking, how long does someone have to follow that for?
Well, once again, that’s why I sort of put more of an urgency on acting on fixing the epithelium as quickly as you can. Sometimes that time frame could be up to three months to four months. Which, in the scheme of things I don’t actually think is a long time. Yeah, okay? Because really, the key is we just want to reduce the inflammatory load. We want to reduce the inflammatory load so that we have a better opportunity of what? Healing the gut lining. Because if I’m dealing with a lot of inflammation and so forth, it’s going to make it harder for me to heal that epithelium. And half the time that’s the problem with people. Because they’ve got so much inflammation taking place it’s making it harder for them to heal the epithelium.
And the one thing is, during that time period, I get the person to really work on mitigating the stress response in the body. Okay? So I get them to do things like meditation. I get them to do things like heart math. Okay? Heart math is actually controlling their emotions at night. Because most of the time people are going to bed in what sort of state? In a stressed state. Okay? If they’re going to bed in a stressed state. Okay? Is there a good chance that during their sleeping cycle if they’re actually causing even further damage to the epithelium. Yeah, okay? So people should really, for me, when they go to bed yeah, okay? Is that’s where they should actually practice things like gratitude, care, compassion, appreciation. So they’re actually changing their state and guess what they’re actually helping with? Okay? It’s proven that those emotional states actually help to increase secretory IgA production. Yeah, okay?
So I actually do a lot of work with people to actually put stress management things in place, okay? So that when they finish something like a gut protocol they’re not going to start to deteriorate that gut lining again. Does that sort of make sense?
That’s great. Thank for this Dave. This has been great. We’re going to have a quick break and be back with the one word game. See you on the other side of this one.
Hey folks. Welcome to the show that punches you in the face with information but in a good way. You’re watching and listening to the Wolf’s Den. On iTunes and on YouTube. So if you are watching this on YouTube, please do me a favor and hit subscribe and give it a thumbs up. If you’re listening to this on iTunes, we would be forever grateful if you could leave us a review. And make sure you follow the show. This is episode 12 with David O’Brien and the last, or past 11 episodes have been equally as fantastic and we’ve interviewed the heavy hitters in the fitness industry to give you the very best content available in podcastland and YouTube long-format interviews today. So we’re going to get into this interview.
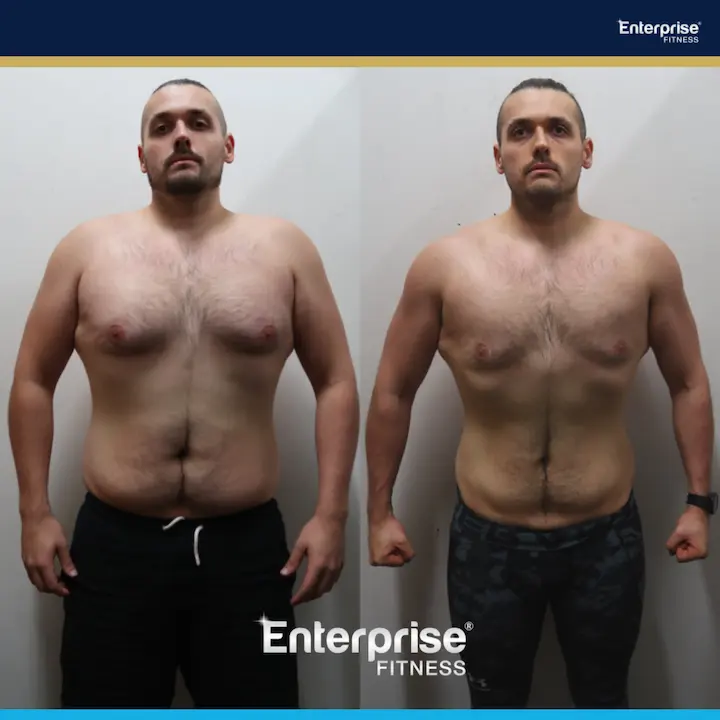
Before we do, I do want to give a huge shout out to our clients at Enterprise Fitness. Our team, our amazing team at Enterprise Fitness. This past Good Friday we raised over $6000 for the Good Friday appeal and the Royal Children’s Hospital. So massive thank you to everyone who came and was a part of it. And yeah, huge, from the bottom of our hearts we want to say thank you.
Now for all the personal trainers out there, do check out this episode that obviously is brought to you by www.personaltrainermentoring.com. Which is your hookup for all things personal training so you can be earning like a superstar and making sure your clients are getting the fantastic results that they deserve. So without further ado, let’s get into the David O’Brien episode which is entitled, “The Gut Show.”
Welcome back to this episode of the Wolf’s Den. We’re with David O’Brien covering all things gut health from dyspoiesis to kombucha. So Dave, let’s get back into the flow. We’re talking about negative gram bacteria. Firstly, what is it?
Yeah, negative gram bacteria just refers to the cell structure of the bacteria. So just so people understand, we’ve got positive gram bacteria which means it has one cell membrane. Okay? And that cell membrane is made of peptidoglycan. Now, peptidoglycan is like amino acids and sugars. Okay? So if you want to understand what would be examples of positive gram bacteria for instance like lactobacillus is positive gram bacteria. Yeah, okay? Bifidobacterium is positive gram bacteria. And what we need to understand is, with positive gram you can have non pathogenic strains, which means they help us with all these different functions and so forth. The interesting thing is, even things with lactobacillus, lactobacillus is a carrier for estrogen so it actually helps to recirculate estrogen through the body. Which means it actually plays a role in helping to clear excess amounts of estrogen out of the body and so forth.
So they can be non-pathogenic in nature or they can be pathogenic in nature which means they can be linked to particular ailments and things like sore throat, sepsis, infections and so forth. Yeah, okay? And then we’ve got negative gram bacteria, okay? And so negative gram, which I’m going to draw now, okay? Its cell structure is a lot more robust. Yeah, okay? And the way that I want you to look at it with bacteria, most of the time bacteria is just taking advantage of a situation. Okay? So if we had a street full of houses, yeah, okay? And then everyone vacated the houses in that street. Generally what would happen? Okay?
Squatters.
Squatters are going to come in. Yeah, okay? And so most of the time bacteria is opportunistic. Which means it’s just taking advantage of a particular terrain or a particular environment. Does that make sense? Okay? And that’s why I put so much emphasis on that particular terrain. And we tend to find overgrowth in negative gram bacteria is really, really common in people when they’re highly stressed, there’s a lot of emotional stress and so forth taking place. Because most of the time we’ve started to deteriorate that epithelium and so forth. Yeah, okay?
But its cell structure, okay? Which I’ve drawn for you before, okay? But its cell structure is: this is the cell, okay? So I’m just talking about one bacterial cell here. Okay? So the key to understand with bacteria, what is the key driver of the bacteria? Bacteria wants to survive. Okay? That’s all it wants to do. Yeah, okay? And it’s highly adaptable, so it adapts to its environment just like we can. It adapts to its environment very easily. Yeah, okay? And so basically, this cell structure that outer membrane, okay? This is what the LPS is, okay? So it doesn’t essentially, the outer membrane is not made of that peptidoglycan. It’s made out of that LPS. Which is the lipopolysaccharides. Which is the fatty acid molecules and the long-chain carbohydrate molecules.
So get a different color, okay? But basically then you’ve got another layer. And that layer is like a periplasm. Okay? And what that periplasm is, is like a gel-like substance. Okay? So you know how you’ve got things like tendon sheaths? Okay? And the role of that tendon sheath is to protect the tendon? Yeah, okay? It’s sort of like another protective membrane. Yeah, okay?
And then, within that you’ve got another membrane. Okay? And this is essentially, that’s the peptidoglycan. So it’s the outer membrane of what you get of the positive gram bacteria, but it’s more internal. Yeah, okay? And once again, that peptidoglycan is amino acids and sugars. Okay? So it looks like that. And then guess what? It’s got another periplasm. Okay? So it’s got another gel-like protective sheath. Yeah, okay? And then, in the middle, it’s got its cytoplasm. And in the cytoplasm is where it forms more LPS. Okay? Because this is an endo-toxin. So when it gets broken down and sometimes when there’s trauma and stress in the body, that can break down the outer membrane. And that gets released into your blood stream.
Now if I’ve got things like permeability and structure issues within the gut? Well guess what? This LPS is going to get into the blood stream, okay? Which is the fatty acid molecules and the long-chain carbohydrate molecules. And could that potentially cause disruption? Because it’s mono-saccharides and poly-saccharides. Could that cause disruption to things like blood sugar and so forth? 100%. That’s why negative gram bacteria has been linked to having really, really elevated things like fasting insulin and maybe the fasting glucose isn’t a problematic thing. But the fasting insulin is through the roof because it’s actually a sign the LPS has potentially damaged things like pancreatic B cells. Which is affecting the release of insulin into the body. Yeah, okay?
So we tend to find, when I look at blood markers, I can see that potentially people have got negative gram bacteria issues because their fasting insulin has actually been disrupted. It’s just one indicator. Just want to clarify that. I use many more indicators than that. Yeah, okay?
And in that cytoplasm, when that bacteria, when the outer membrane gets broken down, then the bacteria forms more. And I just need people to understand, this is not necessarily a bad thing. It’s just, once again, if you’ve got an overgrowth then too much LPS is getting released into the system. Okay? But when that endo-toxin gets broken down, it forms more LPS in the cytoplasm. Helping it form another membrane. Okay? But what I need people to understand, when it comes to negative gram bacteria it’s adapted. Okay? It’s adapted to its environment and us bombarding it with things like antibiotics and so forth. Well guess what? Now it has another protective membrane. Okay? And that’s essentially what we call a biofilm. And we’re finding that more and more things like yeast and candida and strains of negative gram bacteria more and more of them have this biofilm. Okay?
And this biofilm is like a sticky, mucal-ish protective lining, okay? And that biofilm contains things like mercury. So things like heavy metals. Okay? But it also contains iron. Yeah, okay? And the whole thing is, I can look at someone’s blood markers, okay? And when they’ve got things like excessively low iron, okay? That can actually be a sign that the negative gram bacteria is robbing them from iron to use it for the protective membrane. Okay? And so what happens is, someone might see that you’ve got low hemoglobin, low iron and they give you iron. We need to understand that iron is highly toxic in the body. Potentially, if they’ve got a microbiome imbalances and gastrointestial issues by you giving them iron, you could actually be making the negative gram bacteria even worse. Okay?
And so what we need to understand is, when we start to break down … now let’s say we start to do an anti-microbial phase where we start to break down this negative gram bacteria, okay? And use a biofilm agent and the biofilm agent breaks down that biofilm. Things like mercury and things like iron, they get released into your bloodstream. You must have the capacity to be able to clear those byproducts out of the system, okay? Because now, it’s sort of like poking the bear. Does that make sense? Because now there’s more iron and mercury going into your bloodstream. Okay? And once again, that’s why you need the protection of things like glutathione. Okay? Because glutathione makes sure that we’re clearing a lot of these byproducts and so forth out of the system. Yeah, okay?
And I tend to find more and more people are having serious issues with things like negative gram, okay? And the LPS cannibalizes the glutathione. Once again, in turn potentially causing issues with things like heavy metal accumulation and so forth. Okay? And things like LPS, okay? And there’s all these different strains of negative gram bacteria, okay? I’ll give you a couple of examples: citrobacter, okay? And in particular citrobacter freundii complex. Okay? That has actually been linked to things like brain abscesses. Okay? Actually things like inflammation in the brain. And actually, a lot of negative gram bacteria and I’m talking about the pathogenic strains, here. Okay? They have been linked to a lot of autoimmune conditions. Okay? Especially like citrobacter freundii complex has actually been linked to MS. Okay?
Klebsiella, okay? And there’s all these different strains of klebsiella under that. Yeah, okay? Well klebsiella has been linked to things like ankylosing spondylitis. Rheumatoid arthritis. Yeah, okay? And so they’ve actually been linked to a lot of serious diseases and health ailments and so forth. And actually, you know I’ve dealt with a lot of people with autoimmune conditions and so forth and actually, one client who I’ve dealt with with MS. I suspected because of the citrobacter freundii complex has been linked to people with MS and guess what? When I did stool testing, what do you think came back? Okay? She actually had overgrowth of citrobacter but also klebsiella. Yeah, okay? And then once again, they are actually linked to autoimmune conditions and so forth.
And they’re also linked to things like pneumonia, meningitis. Yeah, okay? But people need to understand all these things, they’re just symptoms. Yeah, okay? Like, even an autoimmune condition. Yeah, okay? It’s a symptom of something more sinister. Does that make sense? And most of the time, it’s a symptom of things like overgrowth of negative gram bacteria and depletion of the mucosal lining and the epithelium. Okay? And then I would argue that’s a symptom of something else. Okay? And most of the time, it’s probably a symptom of you overloading the HPA access. Like HPA dysfunction.
So everyone, remember when adrenal fatigue was a hot topic? Everyone goes, “Oh, I’ve got adrenal fatigue.” Yeah, okay? And it’s not really adrenal fatigue, you’ve got HPA dysfunction. You’ve basically overloaded the hypothalamus, the pituitary, and the adrenals, okay? And it’s actually generally caused by four factors. Okay? One is poor circadian rhythms. So I believe when Ben was in here he put a huge emphasis on regulation of sleep. 100%.
That’s the Ben Cant episode.
Yeah, okay? Super smart guy and he put this huge emphasis on regulating your circadian rhythms. Okay? So if you want to minimize that HPA dysfunction? Regulate your circadian rhythms in the body. Best way to do that, is impact things like DHEA, you have GABA which is gamma-Aminobutyric acid, yeah, okay? And melatonin. Okay? And just an interesting side note, 400 times more melatonin is produced in the digestive system than in the brain. Yeah, okay?
Wow.
All right. So regulate your circadian rhythms. Another one is regulate blood glucose levels. Okay? You want me to be honest? That’s one of the easiest things to regulate. Yeah, okay? It just means the person’s got to apply it. Yeah, okay? The other one is reduce inflammation. Reduce inflammatory load. And my big thing here, that’s why I put such on the gut because if I’ve got pathogenic strains of negative gram bacteria if I’ve got deterioration of the epithelium is this potentially causing a lot of inflammatory responses and antibody response in the body? 100%. Okay? And so by mitigating that inflammatory response in the gut, I’ve peeled back one of these key layers that is causing this HPA dysfunction. Yeah, okay?
And the other one is perceived stress. Hardest one to deal with. Okay? Why? Because that’s people’s social condition. That’s their belief system. And a lot of the time when I’m healing people’s gastrointestial issues because they’re not doing the work when it comes to that perceived stress, okay? What do you think is going to happen again? They’re going to start to deteriorate the epithelium they’re going to start deteriorating the gut lining. And this time they just get some sort or other bacterial issue. Does that make sense? Okay? And so I don’t want people to get me wrong. I’m not saying you heal your gut and all your problems are fixed. Yeah, okay? But I’m telling you, if you heal the gut lining, you’re peeling back one of those big layers. Because if I’ve got gastrointestial stress and the bacteria’s releasing a lot of these byproducts and so forth, is there potential that that’s causing more pressure on the brain? Yeah. Because it’s overloading the HPA access. Okay?
But if I peel that back, now I minimize that pressure on the HPA access. Which means now the person is in a far better place to start to do work on what’s going on in their brain. Does that make sense? Yeah?
Very good. Very good. All right, I think it’s now time to move to what we always do on this show which is the one word game. So the way it works for those who are new to it, is let’s say for example I would say something like, “Superhero.” And you might say, “Iron Man.” For example. So it can be one word or it can be a phrase.
Okay.
But we’ve got to keep it sharp.
One word scares …[crosstalk 01:17:43]
Ready?
Obviously people listening to this podcast [crosstalk 01:17:46] is going to test me, yeah?
One word or phrase. All right, ready?
Yep.
Yep. Spirit food.
Liver.
I think you’re the only man in Australia who would say liver. How do you cook your liver? And who’s liver?
You just slightly pan fry it in butter. So you’re getting a lot of that buterate. Liver, this is longer than a one word.
That’s all right. You said it. [crosstalk 01:18:12] I went into the hole myself.
The whole thing with liver, if I had to pick one food that is the most nutritionally dense food known to man? Is liver. [crosstalk 01:18:19]
Undisputed. But it tastes disgusting.
[crosstalk 01:18:23]
Are we talking like beef liver?
Chicken liver, yeah.
Chicken liver. Is that your choice?
Beef, like calf liver is pretty good as well. I know I’m going to freak people out. Just understand the whole thing with offal and organ meats, it’s social conditioning. Most people when I say, “I need you to eat a little bit of liver, lamb’s brains.” They just screw up their nose. And I go, “Oh, you’ve tried it before?” And they go, “No, no.” I go, “Well how do you know if it … that it tastes bad?” Okay? So most of the time it’s the social conditioning. And the fact of the matter is if … [crosstalk 01:18:51]
Dude, I’ve tried it before. I’ve had it many times. I’ve tried eating it. I’ve got the whole 20 kilo cow’s liver in the fridge and it’s just like, “Ugh.”
But it’s a storehouse. So it’s got a lot of things like fat soluble vitamins, vitamin A, vitamin D, vitamin E. A lot of omega-3 fatty acids. [crosstalk 01:19:09]
I agree.
Cholesterol, iron.
Just need to get a chef to make it taste nice. All right, next: comfort food. And if you say liver …
Potatoes.
Oh, there we go. Gluten.
Depends.
Go-to supplement.
Magnesium.
Supplement you can’t live without.
Glutathione.
Book you recommend.
Why Doesn’t my Brain Work? By Dr. Datis Kharrazian.
A podcast you listen to. The Wolf’s Den. A podcast you listen to.
Guy Laurence’s podcast, actually.
What does he do?
He’s more about what’s going on internally in the brain. So he has people on there like Bruce Lipton, Gregg Braden, okay. Because obviously, I just think that’s the area that a lot of people are … it’s sort of like the icing on top of the cake.
So are you talking about neurotransmitters kinda stuff or are you talking about …?
Belief systems and people’s social conditioning. Their emotional health. Because as I said, I’m just finding, because that’s not my specialty and as I said …
What’s that one called?
The Guy Laurence Podcast.
The Guy Laurence Podcast. Recommended movie?
Captain Fantastic, actually.
Captain Fantastic. What’s Captain Fantastic?
I’m getting a few more questions out of you here.
Yeah, yeah.
Captain Fantastic is basically based on a family that go off the grid. Yeah? And it tackles that sort of conundrum of the good aspects or that and then the bad aspects of that in terms of not having social interaction. I just think it’s a good indication of having a bit of blend of that.
Right.
Which I firmly believe is what we need to go a little bit more towards.
Bit off the grid, bit non off the grid.
Correct.
Half, half. Interesting. Someone you admire.
There’s many people. I’m going to go, because I could go really standard with this answer but my best mate Paul Hubber. Unfortunately he passed away before I opened the gym. But I admire him every single day.
Awesome. A person who’s been a mentor to you.
Look, Charles had one of the biggest influences on me. So I’m going to have to say Charles. Even though I’ve had many and some amazing mentors. But Charles, yeah, been huge.
Something you would like to see more of.
I would like … this is not a one word answer, yeah?
Yeah. Well, depends on how your brain thinks.
Variation.
Variation. Less of. Something you want to see less of.
Oh, that’s good. People thinking that there’s one solution to everything.
Food everyone should avoid.
Stuff that’s been genetically modified. Tampered with. That’s what it comes down to. All food’s good until we’ve tampered with it. Dairy’s amazing for you. You know? Pasteurized dairy, homogenized dairy’s terrible for you.
Agreed. Something that you’re excited about.
I love my job. Love it.
Most common … just actually, before I move on from that one. What is your job?
I was asked this question, can I speak on that?
Yeah, yeah, yeah. Oh yeah.
Okay. Someone asked me a good question on a podcast once and they said, “If you were in a plane with someone and they asked you what you did, what would you say?” And typical answer would be you say you’re a personal trainer. But I would say I’m actually a generalist. And actually, if you want to ask my opinion how we’re actually going to really make a big difference in people’s lives? Is, I think, in this industry we need to be more of a generalist.
Very good.
Yep.
The most common health issue you see.
Gut issues.
If you were an exercise, what exercise would you be?
Charles is going to hate this, but I’d say maybe doing squats on a bosu pad. It’s a bit of a mix.
A resource all trainers should have.
Books on many different realms.
And finally, complete this sentence: It’s time for …
To fix your gut.
Nice. Very nice. Let’s give Dave a round of applause. All right. We are going to go to audience questions and the first question is from me. I’m going to pretend to be a part of the audience, but I didn’t get to get into this topic and I do want to get into this topic just quickly with you. And that’s cold therapy. So if we can just, for the camera I suppose we have to discuss this before. But the difference between, you know you see those crypto-chambers or whatever people are going in super cold versus what you’ve been doing down that 5th Element. Can you talk a bit about that?
Yeah, look. I was asked the question once if I was to pick one thing that actually has some of the most biggest biochemical benefits in the body, I actually would pick ice therapy. Okay? Now, whether that was going to be the case 200 years ago? Possibly not. Okay? But because so many people are immuno suppressed, they’ve got so many inflammatory responses I really do think ice therapy is going to come to the fore. Okay? Because … and people need to understand, for me doing things like doing it through air like actually doing the chambers and so forth, it tends to be people that just don’t want to get in the ice water. Okay? Now air conducts completely differently to water. Yeah, okay?
So the whole thing that we need to understand when we’re doing something like cold water ice therapy, yeah, okay? Initially what happens is you actually cause vasoconstriction in the body. Yeah, okay? So you actually minimize blood flow to the extremities like the arms and the legs and so forth. And a lot of people are going to go, “Well that seems terrible.” Yeah, okay? Because obviously, you want to protect the vital organs, okay? So you want to protect things like the heart and so forth. So you’re going to keep a lot of that warm blood flow around the vital organs. Yeah, okay? But actually when I get out of the ice. Yeah, okay? You actually … blood rushes to the extremities. Yeah, okay? And that actually causes high amounts of vasodilation. Yeah, okay? So you actually cause a thing called flushing. Okay? Which means, it actually helps with things like transportation of oxygen and nutrients around the body and so forth.
And also, you need to understand if I’ve got someone who’s immuno suppressed, which means their white blood cells are down their neutrophils are down, their monocytes and their lymphocytes. There’s nothing more powerful for fighting off all this stuff that I was talking about than your own immune system. Okay? And guess what? When you get in the ice, okay? Causes a stress response. Okay? Which means your body, when you have a stress response, you’re going to stimulate your immune system. Which means that’s why they’ve actually recorded an increase in things like neutrophils and lymphocytes and when we’re increasing the production of these things, then they’re going to actually help to fight off a lot of these microorganisms and so forth.
But also, on top of that, inflammatory load. Yeah, okay? So a lot of people’s problems are, is that they’ve got a lot of pro-inflammatory in the body. Which means the body has to produce more antiinflammatory mediators to combat that. Yeah, okay? Which takes a lot from the body. Remember I talked about things like prostaglandins and that which is really taxing things like your omega-3s and so forth. Yeah, okay? Now, if I get in the ice that brings down pro-inflammatory activity which means your body doesn’t need to do what? It doesn’t need to produce antiinflammatory mediators to combat that. Yeah, okay? Which means I’m bringing down inflammatory load. Okay? If I bring down inflammatory load in the body, you’re giving the body the opportunity to do what? To actually healing mechanisms in the body. Yeah, okay?
And the other thing is, I think it’s just completely underrated when it comes to fat burning. Okay? Because it’s all to do thermogenesis. Yeah, okay? And actually, just to understand, I’m big on nutrition and obviously training and so forth. But it can be quite slow when it actually comes to helping with things like fat burning and that. But trust me, when you get in the ice? Yeah, okay? Your body has no choice. So if you’ve got things like leptin resistance and insulin resistance, okay? The body in that instance is not going to go, “Well we’re not going to generate heat.” Yeah, okay? You sit in ice, that actually causes you to stimulate things like brown fat. Okay? And I actually find a lot of people who have got issues with brown fat because your high brown fat stores are around areas where you’ve got high metabolic activity. Like around areas like your thyroid. Okay? Your liver, your kidneys and your adrenals. Let’s look at what people are suffering like hypothyroidism, hypocortisolemia. They’ve got poor liver function. Poor kidney function. And that’s probably what they’ve got poor brown fat stores, okay?
Now just to understand, when you get in the ice. Yeah, okay? You’re going to have to generate heat, okay? Which means you’re stimulating more brown fat. Which is high in mitochondria. Which basically means you stimulate a protein called UPC-1 which is uncoupling protein. Which means you’re taking fats and sugars and you’re converting them into what? Heat. For me, it’s completely underrated. Yeah, okay?
I was thinking, you know what we should invent? You know those tummy trimmers? You know people will sit there and they’re like, “Oh, I’m losing weight.” We should do that but in ice water. Because then it actually might work. Might actually work, you know? It’s going to do something. [crosstalk 01:28:54]
For it maybe. We can go into business you and me.
I just want to sit back and lose fat and not do anything. I just want to lose in my sleep. Yeah. Just, either way. Just sit in cold water and … I just want to see someone who would buy something like that. A person who would buy the tummy trimmer sit in some cold water and just be like, “Yeah. I’m losing fat.” That’d be like … [crosstalk 01:29:12]
I tell you, ice therapy is a hard sell.
Yeah.
Okay? But I don’t think there’s anything more indicative or reflection of life itself. Okay? Because most of the time, the best things in life there’s a bit of short term pay for a long term gain. Okay? You get in the ice there’s a short term pain there, but then that long term gain of reducing the inflammatory load, helping with things like fat burning, helping with those things like uncoupling protein, helping with things like PGC-1 which helps with mitochondrial density. Okay? There’s this huge array of biochemical benefits. Yeah, okay? But you have to go through a little bit of this short term [crosstalk 01:29:51]
You guys do it once a month down at 5EW? [crosstalk 01:29:54]
I went through a stage, I think it was a little bit of ego. Yeah, okay? I just wanted to see if I could get up to Wim Hof standard. Yeah, okay? Because he’s obviously done like one hour 56 minutes actually in ice. Me and one of my clients, Mark, we actually got up to 30 minutes at one degree. Yeah. I was pretty keen to keep on going but Mark just couldn’t. There’s a bit of an afterdrop, when the blood’s actually going back into your extremities and that. And it’s actually quite painful, yeah? But actually …
What do you mean? Hang on. Back up. What do you mean it goes back into your extremities?
So basically, because you’ve obviously … you have to protect your core temperature. Yeah, okay? So when actually start moving again and so forth, the blood’s rushing back into the extremities and actually that feeling of flushing can actually be quite painful in the lower extremities like your fingers. More your hands, to be honest. Yeah, okay? And actually, most of the time you’re actually sitting in the ice and you’re just thinking, “I wouldn’t mind just staying in here so I don’t have to feel that.” Yeah, okay? Actually, once you get past the first minute and a half, two minutes in the ice? It’s easy. Okay? Because the end of the day, it’s just like training. Yeah, okay? The body’s going to do what? It’s going to adapt. Okay? And it’s just the fact that people … it’s a good stress on the body. It’s asking your body to adapt. Yeah, okay?
And that’s why in the middle of winter … people need to understand, Melbourne’s not cold. I never wear a jumper, okay? Because actually got good blood flow, good circulation. Good thermostat. Yeah, okay? I’m actually able to regulate my body temperature. And people just go, “Well you’re shivering. That’s bad.” I’d argue that til the cows come home. When you’re shivering that is your body generating heat. Let your body generate heat. Let your body do what it’s good at. Most of the time we’re taking it away from doing what it’s good at. Yeah, okay? And then guess what? You’re not going to be great at taking sugars and fats and then converting that into heat and energy.
Sensational. Sensation. All right. Now we’ll actually turn to the audience for questions. So our first audience question is from Beck.
Hi.
Hi Beck.
I just wanted to get your gist of … a gen prop client walks into your studio and just, run through it. I know it’s going to be very general topic, but your process of nutrition, stress, training. What is your basic protocol?
Yeah.
Straight up.
Basic protocol because, I think for me I just don’t deal with general pop so much anymore. Yeah, okay? Because basically, the people who come to me have got serious ailments and diseases and they’re actually in a position where they probably don’t have too much choice. Does that make sense? So normally I’m looking at their bloods and I’m [crosstalk 01:32:24] yeah, going straight into something like epithelium repair and intestinal permeability repair and all those types of things.
But, look, I would generally say based on what I’ve been talking about today is I would start to apply things that are actually going to help with that structure of that gut lining and so forth. Yeah, okay? So giving them something like zinc. Yeah, okay? Because for the epithelium you’ve got an ingredient. Yeah, okay? And the ingredient for that epithelium is zinc. Actually, vitamin B6 which is pyridoxine that’s why something [crosstalk 01:32:55] zinc l’carnosine is generally better because it’s bound to a antioxidant. Yeah, okay? Or like an amino acid. Okay? So it allows the zinc to stay around longer in the gut. Yeah, okay? So zinc l’carnosine yes. At the moment, because people have got so many gastrointestial issues. I don’t think it’s the best zinc. Okay? But when you’ve got gastrointestial issues. It helps with peptic ulcers, and H. pylori and SIBO tends to be taken better in the gut. B6 as well, but I’m not necessarily saying you have to get that out of taking something like a P5P. Okay? Pyridoxal phosphate. Because maybe you include a little more B6 in your diet and guess what? Things like scallops and potatoes are actually really high in B6. Yeah, okay?
And prebiotics. But the problem with prebiotics … Yeah, okay? Is generally they can actually feed the bad bacteria. They feed the negative gram bacteria and so forth. Yeah, okay? But also, particular amino acids like things like arginine and glutamine. And guess what’s quite high in things like arginine and glutamine? I prefer to go with things like slow cooked meats in that instance. Yeah, okay? Actually prefer to go a little bit more initially with fatty meats. Okay? Because they actually help with things like glycine, arginine and proline. Yeah, okay? Which means they’re also helping with things like synovial fluid and hyaluronic acid so they’re helping people move and so forth. So slow cooked meats is a generally an easy win. Yeah, okay?
So I’m looking at some things that will help with the epithelium but also things that will help to not damage the epithelium. Yeah, okay? So I apply things like meditation. Yeah, okay? Now, I’m not going to get into the complexities like metacognition or all that, but just get them to meditate every single morning. Yeah, okay? Doing something like heart math at night. Because most of the time, people are looking at things like adaptogens and all this type of stuff. Just control people’s emotional stress at night. Get them to go to bed. That’s where they should close their eyes down, put their hand on their heart. It’s actually called heart math: left hand over the top of the right hand, close their eyes down and think of what they’re grateful for. Yeah, okay? Gratitude, care, compassion, appreciation. And guess what? Now you’ve changed their emotional state.
These are big wins. Because that’s also going to affect their heart rate variability. Which is a time fragment between beat to beat. Yeah, okay? It’s one of the quickest ways to impact heart rate variability. Things like oxidation, long term system and like a steady state and that’s slow. Yeah, okay? It’s changing their emotional state. Because now they’re going to have better sleep. They’re going to have better circadian rhythms which means they’re going to help to repair their gut lining and all this type of stuff. Yeah, okay? I know for a lot of people that stuff seems fluffy, but I’m just telling you. And getting them to probably have a cold shower. Yeah, okay? Cold shower’s an easier win than chucking them in an ice bath. Yeah, okay?
But for me, I want to go for things that have the huge cascade effect in the body. And even when it comes to micronutrients. We go too complex. Okay? Can’t beat vitamin C. But don’t get an ascorbic vitamin C, get like a natural vitamin C. Like a kakadu plum. Yeah, okay? Because the body recognizes it better. Vitamin A is a no brainer. Yeah, okay? Because that’s what you need for your stem cells, it helps with your white blood cells. Yeah, okay? Like I don’t know why we’ve gone for these specialized supplements and so forth. I want things that are cascade effect in the body. They’re going to have the biggest chemical reactions. Yeah, okay? More cascade effect I get in the body? Guess what? More biochemical changes in the body. More rebalancing of the body.
Thanks for the question, Beck.
Yeah.
I guess my question was about diet and chemical stressors versus emotional stressors. And so do you find that you’re having to calm people down when they’re focusing so much about the minutia of their diet and little things because they’re getting so worked up that they’re not hitting their macro or micronutrients for the day?
Yeah. It’s a good question. Because believe it or not, when it comes to things like macroplans and sticking to a particular food plan and so forth, you know I’m going to be honest, I am a big advocate of that. Okay? I’m not talking so much about body composition here. Yeah? I’m talking about I actually use it as a healing mechanism in the body. Because most of the time these people are completely malnourished. Yeah, okay? They’re missing a lot of the key macronutrients and micronutrients. And me just telling them to eat these certain foods might not still be enough. Yeah, okay? It might not be enough to help with things like their sex hormones and their thyroid and all that sort of stuff.
So I think those types of things, it’s the way you communicate that with people. Does that make sense? Because a lot of the time. Yeah, okay? If you explain to them that it’s having these healing mechanisms in the body, it’s not going to stress them out so much because they realize it’s going to help with their cognition, it’s going to help with their brain function. More, for me, is how we’re delivering this information to them. If you deliver in a way that they understand that it’s going to benefit their everyday life and it’s going to benefit the things that are really high values for them? Yeah, okay? I’m telling you, give people good reasons to do things and it does not stress them out. Give them a poor reason to do something and they’re going to be stressed out.
[crosstalk 01:38:03]
100%. It’s the delivery that is the most important thing in that.
Perception.
Yeah. Perception. Okay? And as I said, people say to me, “Why do you go so technical? Why do you talk about so many technical elements?” Because if I turn around and tell someone they need to eat more fats because fats are really good for your cells. What does that mean to them. If I give them a list of all the different reactions: that it’s going to help with their steroidal hormones. Yeah, okay? Their brain is basically made up of saturated fat. Yeah, okay? That saturated fats are needed for your white blood cells because, especially things like myristic acid and lauric acid they help your white blood cells recognize pathogens and microorganisms. All of a sudden, they might not remember any of that. Yeah? True. But now, they’ve got huge significance on that. Does that make sense? Now they’ve got huge significance which means when people have got huge association with how important it is? What do they do? They do it.
Awesome. Thanks for the question. Liam, sir.
Thanks David. I [inaudible 01:39:11] about the inflammation matters. If you don’t research more than me in the room. But my question today was sugar and artificial sweeteners and obviously affecting leaky gut and therefore leading to potential body fat gain. Can you give me a breakdown of how artificial sweeteners actually lead to gut damage and excess body fat gaining? If it does?
Which artificial sweeteners are you talking about? And …
Well there’s more in the high FODMAP area. Like the ones that are found in juices.
Like Stevia [inaudible 01:39:48]. What others?
Sorbitol. Even honey, for example.
You’re looking at a lot of the good sweeteners that are obviously come into the fore which are more based on the low FODMAP realms like things like maple syrup. Yeah, okay? And the good thing about something like maple syrup’s so high in trace minerals and so forth. When I look at sweeteners. Yeah, okay? This is what people should be doing: you should be looking at it and say, “What does it give my body?” Okay? Now, if I look at Stevia, so don’t get me wrong, I’m not disputing the science on Stevia. Yeah, okay? And yes, it doesn’t have the same kind of negative impact on your blood glucose levels. Yeah, okay? But then the science isn’t conclusive but we can say that Stevia potentially might cause a little bit of disruption with some microbiome imbalances and so forth. Yeah, okay? But it’s not necessarily conclusive. Yeah, okay? But I do tend to find when I give people, if people have things like Stevia and they’ve got things like negative gram bacteria and SIBO, it tends to aggravate their gut. Yeah, okay?
But I really encourage people, when it comes to sweeteners, is identify what am I getting out of these sweeteners. Yeah, okay? And honey, for me is a good natural sweetener because it actually helps with beneficial enzymes, it’s got antibacterial benefits and so forth. But then, the fructose can be a problem for when people do have actual bacterial issues. And once again, but that’s not the problem of honey. Does that make sense? Yeah, okay? Sometimes it’s the quality of honey that can be an issue because it’s got high fructose corn syrup and so forth, because it’s been sort of cross bred and so forth. Yeah, okay? But I’d say it’s more the issue with your gut lining. Does that make sense? Okay?
And so once again, if you fix the gut lining and you get rid of the bacterial issues and so forth then you’re not going to face this thing where you’ve got to avoid all these good sweeteners and so forth. Yeah, okay? You got things like rice malt syrup. Yeah, okay? Because rice malt syrup is a good sweetener to use because it’s low fructose. But once again, that’s whilst you’ve got issues with fructose and so forth. It’s a good alternative. Yeah, okay? And things like molasses. Yeah, okay? Because molasses is really high in things like iron and so forth. So I think there’s better alternatives while you’ve got gastrointestial issues but I always look at sweeteners and say, “What am I getting from it?” Okay? And if you’re getting trace minerals and you’re getting things like B vitamins, you’re getting things like … these are the sweeteners that we need … that’s how we need to look at food. Yeah, okay? We need to look at, “What am I getting from it? How is it might benefit my body?” And what I’d argue is things like Stevia and xylitol what am I getting? What am I getting that’s actually going to benefit my body and so forth. And if I’m going to get all these other amazing properties from things like maple syrup and so forth, that’s a no brainer. Does that make sense?
Great. Very good way to put that. Yeah. Very good. Are you adverse to the artificial sweeteners?
Once again, I just educate the people with what are we getting from it? That’s what I think people need to look at food.
Rather than be the three year old of “That tastes sweet and I’m just substituting and food’s supposed to be sweet.”
If there is some bacteria in your gut lining and you are having carbs which end up being sugar anyway.
Yeah.
So they’re feeding bacteria.
Which would be more problematic for things like yeast and candida and particular parasites like blasto, like blastocystis hominis and dientamoeba fragilis and that because they do feed on carbohydrates. But understand, a lot of negative gram bacteria is fine on carbs. Okay? It just tends to be the FOSs, the fructooligosaccharides like things like onion and garlic and leeks and artichokes and wheat and barley. Does that make sense?
Yeah. It’s almost where you come back to there’s no real wrong foods, it’s all about what’s happening in here. So I don’t know if it’s glucose or high fructose corn syrup. Still going to affect.
Yeah. Exactly. Just got to get away … like people saying that meat is bad. Poor quality meat is bad. Meat’s exceptionally good for you. And I would argue a lot of people have been turned off by animal protein and I’d argue they’ve actually got things like H pylori and hydrochloric acid issues because guess what? If you’ve got hydrochloric acid issues.
You don’t eat meat.
Yeah. You’re going to be off put by the thought of eating meat. Yeah, okay?
Because you can’t digest it.
And so the body’s sort of intuitive in that way. It just goes, “This is quite a taxing process on the body.” Yeah, okay? And I’d argue the number one probably reason they’ve got hydrochloric acid issues in the stomach is because they’ve got poor energy systems. They’ve got poor ATP production and if they’ve got poor ATP, then they’ve got poor byproducts like things like carbon dioxide. And carbon dioxide mixes with water in the body to form bicarbonate. Okay? And bicarbonate is one of the key building blocks that I need for hydrochloric acid. Okay? So you could say that they’ve got the poor energy system. Yeah, okay? Then they’re producing low levels of hydrochloric acid because they’re not getting enough things like carbon dioxide and so forth. And then that’s going to affect how they’re breaking down things like animal protein. And they go, “Oh, the animal protein makes me feel sick” And so forth. And I go, “Yeah, but that’s an issue in your digestive system.” And you’ve actually taken out a food group based on the fact that it’s hard to break down and so forth and it’s the same things with like fats.
Because if I’ve got problems with the epithelium that affects things like micellizing factors which actually help with fats and oils and so forth. Yeah, okay?. And then they just go, “Well it feels hard in my gut.” And so then they’re going to eat more carbohydrates. Okay? But it’s not a problem with the fats. It’s the same thing when people have got things like their bilirubin might be really really elevated which can be a sign of fat metabolization issues. You have fat malabsorption and then we look at that and that’s the problem when you look at things and you’re just basing it on what’s going on in that moment and time. Yeah, okay? And then they go, “You should eat more carbohydrates. And you shouldn’t eat as many fats.” And I would argue, actually the reason they’ve probably got the elevated bilirubin is because they’ve got a build up of the bilirubin in the blood stream because the bilirubin is not actually getting processed in the small intestine properly. Because they’ve got something like SIBO. Like small intestinal bacterial overgrowth. And what’s the worst thing you could potentially give the person in that instance? More carbohydrates.
Absolutely.
You actually cause a bigger problem. Do you know what I mean? So this demonization of food needs to stop. Stop demonizing dairy, stop demonizing fruits, stop demonizing whatever. Because most of the time it’s the quality and it’s the problem with the area that has to assimilate it which is your digestive system. One thing that I didn’t bring up which I think is a great analogy. If I had a waterfall and I said to you, “Mark. Yeah, okay?”
TLC. Waterfalls. Don’t go chasing them waterfalls.
If I had a waterfall and I said to you, “Mark. Why isn’t this waterfall flowing properly?” What part of the waterfall would you go to to find out why it’s not flowing properly?
Well, obviously the bottom. No. Obviously the top.
It’s the top. And when I say the top of the waterfall is food. It’s the quality of the food that you’re putting in your body. The middle section is the area that has to assimilate it, it’s like the filing cabinet. It has to help us produce these particular compounds, like protein compounds and neurotransmitters and hormones and so forth. And the bottom is the byproducts. It’s the neurotransmitters, it’s the hormones and so forth. And guess which area of the waterfall we’ve been stuffing around? The bottom of the waterfall. We’ve been stuffing around the byproducts. And I’m not saying they’re not issues. Because with a lot of people, they can have genetic mutations, 100%. I’m not denying that. But if I want to have the biggest cascade effect in the body? [crosstalk 01:47:26]
Top.
I’m going to look at the quality of that food. And I’m going to look at the area that is the filing cabinet that has to sort it.
So Dave, this has been epic. Thank you. Thank you. [crosstalk 01:47:35]
No problem, mate.
It’s been a real pleasure. [crosstalk 01:47:37]
It’s been an honor.
We’ve got to do this again sometime.
For sure.
Where can people learn more about you?
Yeah, well I’m not big on Instagram. I am going to get on there eventually. Yeah, okay? But look, 5th Element Wellness, which is 5EW.com.au Yeah, okay? Look, I do take a lot of seminars, I take seminars on gut health. That’s probably the realms that I’m going more and more into. It’s a seminar called It’s All About the Gut. Even a little bit further down this rabbit hole. Yeah, okay? But a lot of the remedies that I’m bringing in to how to fix these issues, I think a lot of the things that I’ve talked about is complex today but the things we can do to fix it? They’re not complex.
Yeah. I’m pretty syked. I want to bring you and Ben Cants. In the Wolf Pack. Put you in the same room together and just shoot the shit. I think it’d be dynamite. So we’ll make that one tee’d up in August if we can. I’ll speak to Ben and you and see if we can do that.
I’ve got the biggest respect for Ben and the industry. He’s doing amazing stuff. Yeah.
So thank you Dave, for the interview. This has been the Wolf’s Den with David O’Brien. This is episode 12. 12? 11? 12? Not even sure what we’re up to anymore but thank you for watching. As always, remember to subscribe on YouTube. Listen to us on iTunes. And if you could, leave us a review. It means a lot to us and a much more than you can know. So til next time, folks: supplement smart, eat well, and train hard.
See you guys.
I hope you enjoyed this episode of the Wolf’s Den with David O’Brien. Hey folks. Are you in Melbourne? If you’re in Melbourne, we would love to have you at Enterprise Fitness in the shooting of the next Wolf’s Den episode. So it’s 381 Swan Street in Richmond. That’s my home, Enterprise Fitness. And we shoot these episodes live in front of a studio audience. So we take a $10 donation at the door. The donation goes to Royal Children’s Hospital. So we donate all the proceeds to the Royal Children’s Hospital and you’re welcome to come along to the next one. So when to know the next episodes the are coming up, the best place to know is to head over to my Instagram account. Hit follow and you get all the updates of new episodes and guests that I’m going to have in the studio. So til next episode: train hard, supplement smart, and eat well.
Related Posts
- Inside the Mind of Ed Coan | The Greatest of All Time
- Understanding Womens Hormones | Coach Jake Carter on the Wolfs Den
- Using Lab Tests for Better Body Composition | Ben Cant on the Wolf’s Den